
Blog
Oops! This content is hosted in another place.
Find it HereType 2 diabetes is one of the most expensive chronic conditions in the United States, driven by high medical utilization and rising prescription drug costs. For employers and health plans, managing diabetes care often means balancing medical care, medications, and lifestyle support.
A claims-based analysis of a large U.S. employer shows that Twin Health’s metabolic health benefit can deliver lower costs and better health outcomes. In the first year alone, Twin reduced total diabetes-related costs by an average of $9,047 per member.

A look at real employer outcomes
Medical and pharmacy claims data from 228 commercially insured employees with type 2 diabetes were evaluated across a 12-month period before and after participation in Twin. Claims were compared with a matched control group using an industry-standard difference-in-difference methodology.
Claims data included:
By evaluating both medical and pharmacy claims, the analysis captured the impact of integrated care on utilization and total cost of care.
The results: lower costs without cost shifting
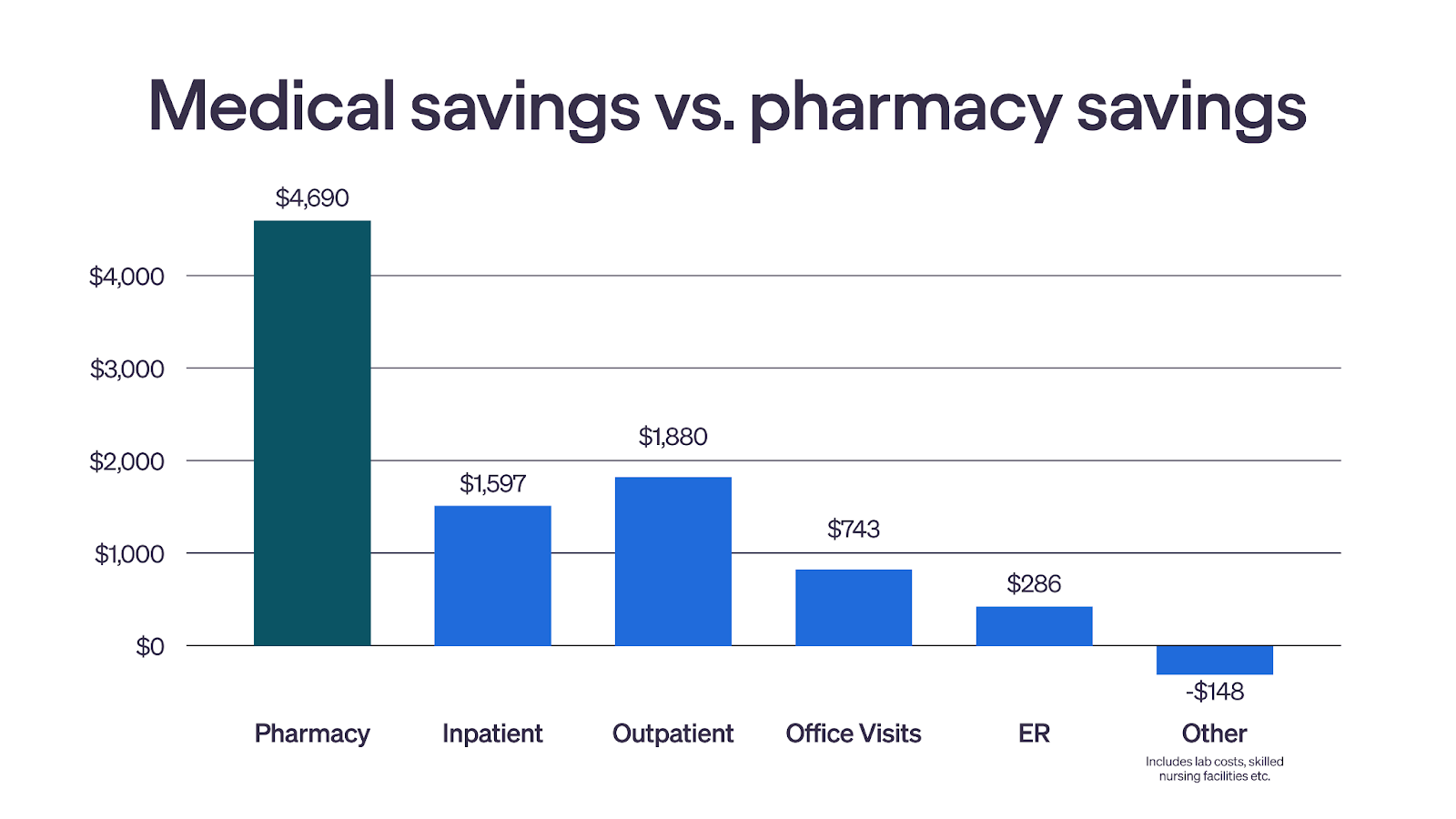
Total diabetes-related costs declined in both medical and pharmacy spend. Savings were driven by lower utilization and medication spend, rather than shifting costs from one category to another. At the same time, members experienced meaningful improvements in metabolic health, including A1C, weight, and cardiovascular risk.
Medical savings
Medical cost reductions were driven by fewer inpatient admissions and emergency room (ER) visits, with $4,357 annually in medical savings per member.
Fewer acute events and complications contributed to lower medical spend, which represents one of the largest drivers of diabetes-related costs.
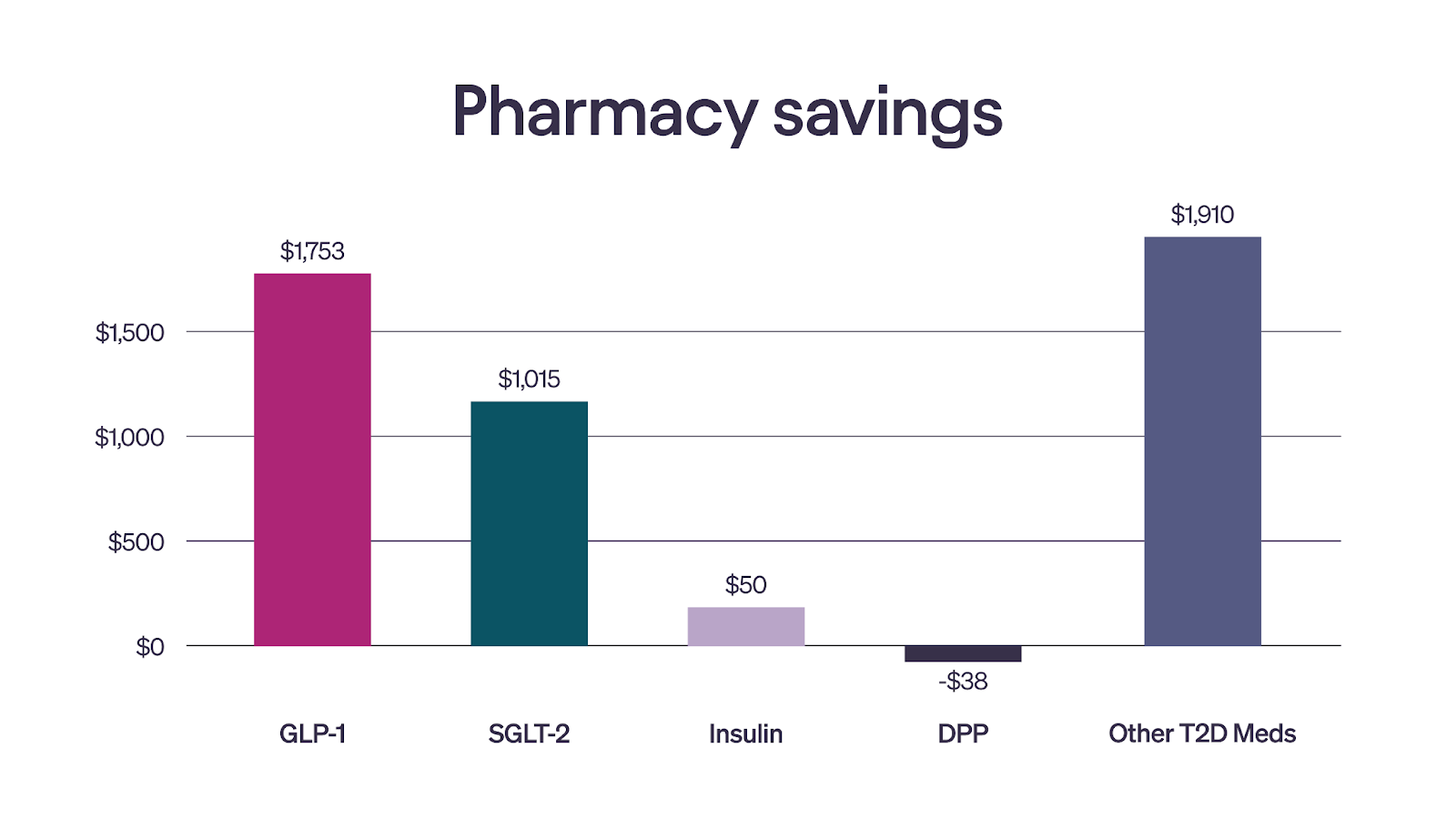
Pharmacy savings
Pharmacy savings reflected reduced reliance on high-cost antidiabetic medications such as GLP-1s and SGLT2s, with $4,690 annually in pharmacy savings per member.
As members improved their metabolic control, medication needs declined, lowering pharmacy spend without restricting access to care.
Why Twin’s approach is different
Most diabetes programs rely on generalized guidance or symptom management rather than addressing the root cause of metabolic disease.
Twin takes a different approach. Each member’s AI Digital Twin creates a map of their metabolism using data from smart devices like continuous glucose monitors (CGMs), smartwatches, and other devices. Paired with clinical oversight and ongoing care team support, members receive personalized guidance that adapts with them over time.
The result is integrated type 2 diabetes care that improves outcomes and reduces costs in a way that is personalized, sustainable, and scalable.
What this means for employers
These findings reinforce an important shift in how diabetes care can be delivered.
For employers and health plans focused on total cost of care, this report provides compelling evidence that a personalized, metabolic care approach can deliver measurable value.
Interested in how these findings could apply to your team?
No content exists for this entry